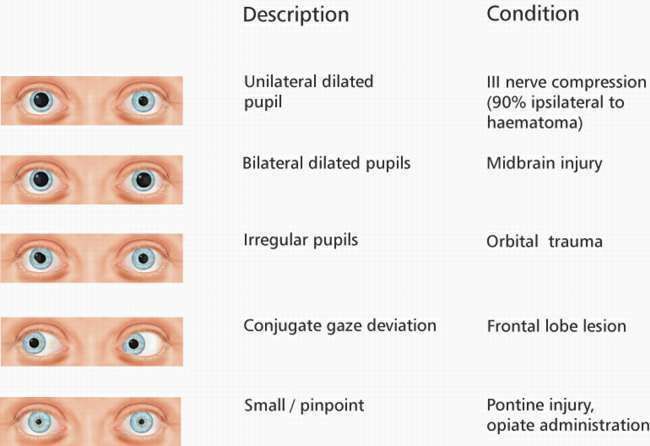
Pupillary evaluation is an essential aspect of a neuro exam, and pupil reactivity plays a significant role in diagnosing neurological disorders. The pupil’s size and reactivity provide valuable information about the patient’s neurological status, and changes in these parameters can indicate underlying neurological conditions.
The nervous system controls the pupil’s size and reactivity and is an excellent tool for assessing the integrity of the autonomic nervous system. In this article, we will discuss the role of pupil reactivity in diagnosing neurological disorders, how it is measured, and the techniques used to evaluate it.
Understanding Pupil Reactivity
Pupil reactivity refers to the pupil’s ability to constrict or dilate in response to light and other stimuli. It is measured by observing the changes in the pupil’s diameter in response to different stimuli, such as light, accommodation, and convergence.
The nervous system controls the pupil’s size and reactivity and is an excellent tool for assessing the integrity of the autonomic nervous system. The sympathetic and parasympathetic nervous systems control the pupil’s size and reactivity types—sensual responses, afferent pupillary defects (RAPD), and tonic pupils. An abnormal pupil reaction can indicate underlying neurological conditions.
Pupil Reactivity in Neurological Assessments
Pupil reactivity is a valuable tool for diagnosing neurological disorders. Many neurological conditions can affect pupil reactivity, including traumatic brain injury, stroke, brain tumors, and multiple sclerosis.
Changes in pupil size and reactivity can also indicate increased intracranial pressure, a common complication of neurological conditions.
Pupil reactivity is with neurological conditions, and changes in pupil size and reactivity can indicate the progression or improvement of the underlying condition.
Pupil reactivity is an essential aspect of the neurological exam. It is often used with other neurological tools, such as the Glasgow Coma Scale, to accurately assess a patient’s neurological status.
Techniques for Measuring Pupil Reactivity
Several techniques are used to measure pupil reactivity, including direct and consensual pupillary light reflexes, the swinging flashlight test, and pupil diameter measurement using infrared pupillometry.
Direct and consensual pupillary light reflexes are the most commonly used techniques for evaluating pupil reactivity. They involve shining a light into one eye and observing the reaction of both pupils.
The swinging flashlight test involves swinging the light back and forth between the two eyes to evaluate the relative afferent pupillary defect (RAPD).
Infrared pupillometry is a non-invasive technique that uses infrared light to measure pupil diameter and reactivity. It provides accurate and reliable measurements of pupil reactivity and is commonly used in critical care settings.
The advantages of infrared pupillometry include its non-invasive nature, the ability to measure pupil size and reactivity simultaneously, and the high level of accuracy and reliability.
However, it is important to note that various factors, such as ambient lighting, medication use, and patient age, can affect pupil reactivity measurements. Therefore, it is essential to consider these factors when interpreting pupil reactivity measurements.
The Future of Pupil Reactivity in Neurological Diagnoses
Pupil reactivity has the potential to become a primary tool for diagnosing neurological disorders. Ongoing research focuses on improving pupil reactivity measurements’ accuracy and reliability and developing new techniques for evaluating pupil reactivity.
One such development is the Neurological Pupil Index (NPi), a new method that objectively measures pupil reactivity and is more accurate than traditional pupil reactivity measurements in predicting neurological outcomes.
Pupil reactivity may also be used with other diagnostic tools to improve accuracy and reliability. For example, combining pupillary evaluation with neuroimaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, could enhance the diagnostic value of pupil reactivity measurements.
Conclusion:
Pupil reactivity is an essential tool for diagnosing neurological disorders, and changes in pupil size and reactivity can indicate underlying neurological conditions. Several techniques are used to measure pupil reactivity, and ongoing research is focused on improving the accuracy and reliability of these measurements.
Pupil reactivity has the potential to become a primary tool for diagnosing neurological disorders, and future advancements in this field could revolutionize the way neurological conditions are diagnosed and treated.
The accurate and reliable measurement of pupil reactivity can improve patient outcomes and enhance the quality of care for patients with neurological conditions. As neurology advances, pupil reactivity will undoubtedly play an increasingly important role in diagnosing and treating neurological disorders.